Breast Reconstruction after Mastectomy: 10 Key Considerations

Today, we’re diving into a topic that’s of immense importance to me and many who’ve faced the challenge of breast cancer: breast reconstruction after mastectomy. It’s a personal decision, and one that often brings a whirlwind of emotions and questions. When I decided to have a double mastectomy, my brain went to reconstruction nearly as much as it did pondering if I would have to have chemo. For many of us, part of our identity may be tied into our female body image. For me, because I feel like I’m not a very girly-girl, it was a mixed bag. I don’t generally feel very feminine and felt like the loss of breasts would make that even harder. So reconstruction was an immediate yes for me. Then I dove into exploring options. I hope this guide helps you as well. I’m following this up with more indepth articles about different reconstruction options as well.
Know Your Options for Breast Reconstruction after Mastectomy
The first thing to recognize is that there’s no one-size-fits-all approach. There are several options for breast reconstruction after mastectomy. You can choose implants, which come in saline or silicone, or flap procedures that use tissue from other parts of your body. Another option is fat grafting. Which route you take will depend on your body type, previous surgeries, and personal preferences.
If you’d like a deeper dive into these options, Cancer.org offers a comprehensive guide.

Saline or Silicone Implants
Saline or silicone implants are a common choice for breast reconstruction after mastectomy. Saline implants are filled with sterile salt water, while silicone implants are filled with a silicone gel that feels more like natural breast tissue. The process typically involves first placing a tissue expander to stretch the skin, then replacing it with the chosen implant. This option is known for its relatively shorter surgery and recovery time but may not feel as natural as other methods.
Silicone implants usually offer a more natural feel than saline ones, but both types have their specific benefits and risks. It’s important to discuss your preferences, lifestyle, and any concerns with your healthcare provider to determine which implant type is the best fit for you.
This is the option I chose, but it was not my first choice, but it became my choice because I could not get scheduled for DIEP Flap Reconstruction within the same medical insurance plan year. I have very high deductible and out of pocket max so needing to put in another $16K in another year was just too much. I hope to be in a place somewhere where I have better insurance and can switch to a DIEP Flap.
DIEP Flap Reconstruction
DIEP (Deep Inferior Epigastric Perforator) flap reconstruction uses skin, fat, and blood vessels from your lower abdomen to create a new breast after a mastectomy. Unlike other flap procedures, DIEP usually doesn’t take the muscle, preserving abdominal strength. The tissue is transplanted to the chest, where it’s shaped into a new breast.
This method offers a more natural look and feel compared to implants but requires a longer and more complex surgery. Recovery can also be more extensive, as it involves healing both the chest and abdomen. The end result, however, can be highly satisfying, as it often ages naturally with the rest of the body.
Goldilocks Reconstruction
Goldilocks reconstruction is a creative approach that uses the patient’s remaining breast skin and tissue after mastectomy to form a new, smaller breast. The name “Goldilocks” refers to the idea that it’s a “just right” option for some, especially those who do not want implants or can’t have other flap procedures.
This procedure is less invasive than other reconstruction methods and avoids the use of foreign materials or additional body tissue. However, the resulting breast may be smaller and less shapely than with other methods. It’s often seen as a middle ground between more complex reconstructions and staying flat.
Staying Flat
Staying flat is the choice to forgo breast reconstruction altogether after a mastectomy. Some women prefer this option for various personal, medical, or aesthetic reasons. Staying flat avoids additional surgeries and potential complications that might come with reconstruction.
For some, the decision to stay flat is empowering. It’s a choice that’s equally valid and beautiful. Staying flat means not undergoing further surgeries for reconstruction, and instead, embracing the chest as it is post-mastectomy. This decision can be influenced by personal, medical, or practical reasons.
Need stories or experiences from those who chose this path? Check out Flat and Fabulous, a community dedicated to supporting those who decide to go flat.
Understanding How Expanders Work in Breast Reconstruction After Mastectomy
If you choose either implants or DIEP flap options, expanders play a crucial role in the breast reconstruction journey. They’re temporary devices implanted under the skin that are gradually filled with saline over time. This helps stretch the skin and create a pocket for the permanent implant. It’s like prepping the space before the final touch! After the desired size is reached, another surgery replaces the expander with the breast implant.
Not gonna lie, for me, the expanders were a real pain in the ass. Mine were put in at the same time as the mastectomy, which was great, and were filled with air equivalent to about a B cup. At my first post op appointment about two week after surgery, they pulled out the air and put in an equivalent amount of saline through a port in each expander. They put some numbing cream on the port spots before they did it and it was very painless, in terms of the actual procedure. For a few days after each fill (I had two more to get me to a full C cup) it was quite achey. As they got heavier, my expanders detached from my chest wall and were moving around. They did rub up against things inside there and as a result of all that, my reconstruction was moved up by a month.
For a detailed walkthrough of the process, the American Society of Plastic Surgeons has a treasure trove of information.
The Cost Factor – How Much Will it All Set You Back?
Cost is, without a doubt, a major factor to consider. While health insurance often covers mastectomy and reconstruction, there could be out-of-pocket expenses. It’s essential to understand your insurance coverage and the potential costs involved in each reconstruction option.
Breast reconstruction after mastectomy can be a costly process, and the expenses can vary widely based on the type of procedure, the surgeon’s experience, the hospital or surgical facility, and the geographical location. Generally, health insurance plans that cover mastectomy also cover breast reconstruction, including surgeries to achieve symmetry with the unaffected breast. This coverage is mandated by federal law in the United States under the Women’s Health and Cancer Rights Act (WHCRA) of 1998. However, individual plans might differ, so it is vital to discuss your specific coverage, deductibles, and potential out-of-pocket expenses with your insurance provider.
For more information about the Women’s Health and Cancer Rights Act (WHCRA) and insurance coverage for breast reconstruction, you can visit the U.S. Department of Labor’s website: U.S. Department of Labor – WHCRA
Options Without Insurance
For those without health insurance or with limited coverage, the financial aspect of breast reconstruction can be particularly daunting. However, options are available to help manage these costs. Some hospitals and medical centers may offer sliding-scale fees based on income or payment plans to make the procedure more affordable. Medical finance companies also provide loans specifically for healthcare procedures, including breast reconstruction.
In addition to the above options, various non-profit organizations and charitable foundations may offer grants or assistance to those facing financial difficulties with breast reconstruction. These groups aim to support individuals going through cancer treatment and recovery, and they may be able to provide support or direct you to resources in your community. Exploring all these options with the guidance of financial counselors, social workers, or patient navigators who specialize in healthcare can help you make an informed decision about what’s best for your financial situation and your reconstruction journey.
Additional Resources:
- The Breast Reconstruction Guidebook has a list of financial resources and assistance programs: The Breast Reconstruction Guidebook
- The Susan G. Komen organization may provide guidance and support related to breast cancer and reconstruction: Susan G. Komen
- The American Cancer Society can connect you with resources and support in your community: American Cancer Society
- For guidance on healthcare financing and potential loans, you might consider exploring medical financing companies like CareCredit: CareCredit
- Some hospitals may offer financial assistance programs, and details can often be found on their individual websites.
Always consult with your healthcare provider, social worker, or patient navigator to identify the best resources tailored to your specific situation and needs.
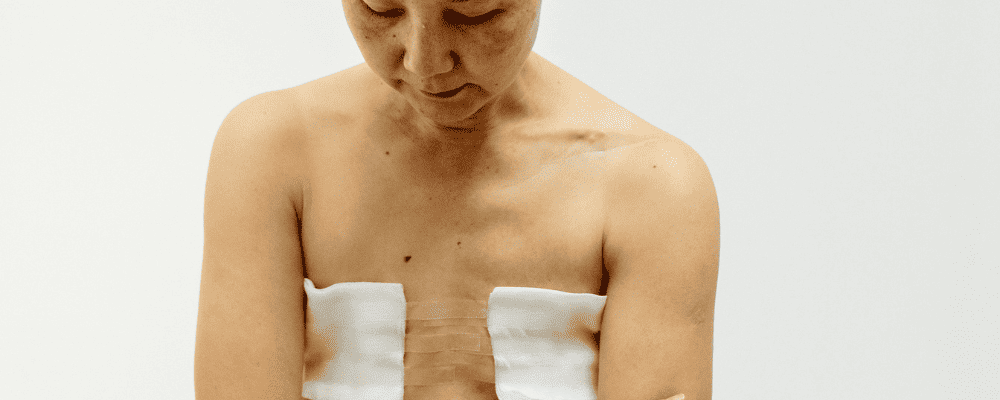
Recovery: What to Expect After Breast Reconstruction After Mastectomy
Recovery varies depending on the type of reconstruction. While some procedures might require a shorter hospital stay and recovery period, others could be more extensive. Knowing what to expect will help you prepare both mentally and logistically.
For tips on recovery, check out my other articles on the specific types of reconstruction, or check out resources like the Mayo Clinic. Mayo is where I had my double mastectomy done, and if you have the means to get yourself there, I highly highly recommend it.
Complications, Risks and How to Navigate Them
All surgeries carry risks. Whether it’s potential complications from anesthesia or the possibility of infection, it’s crucial to understand and weigh these risks against the benefits.
This National Cancer Institute guide provides an in-depth look into potential complications.
The Importance of Aesthetic Outcomes
Reconstruction is not just about replacing what was lost. For many, it’s about achieving a desired aesthetic outcome. This could mean considering nipple reconstruction, tattooing, or achieving symmetry between breasts.
For more on this, The Pink Ribbon Boutique offers insights and solutions.
How Reconstruction Impacts Mental Well-being
Breast reconstruction after mastectomy isn’t just a physical journey—it’s an emotional one too. It’s crucial to acknowledge and prepare for the roller coaster of feelings that might come your way.
For emotional support and resources, check out the Young Survival Coalition.
When is the Right Time for Reconstruction?
You might opt for immediate reconstruction (right after mastectomy) or delay it. Your choice might depend on factors like additional treatments required or personal reasons.
For more on the timing of reconstruction, the Breast Reconstruction Guide offers some perspectives.
Seeking Second Opinions
Remember, it’s always okay to seek second or even third opinions. Each surgeon might offer a different perspective, and gathering various viewpoints can help you make an informed decision.
For tips on how to effectively seek out second opinions, Susan G. Komen has some excellent advice.
Final Thoughts
Whew! That was a lot to take in, right? Just remember, your journey is unique, and so is every decision you make along the way. Whether you opt for reconstruction or choose to go flat, embrace your choice with love and confidence.
You might also want to check out: